How I Learned I Had Iron Deficiency Anemia: ‘I felt like I was dying’
WRITTEN BY CHELSEA C.I don't remember the exact moment I started believing that feeling terrible was just part of being a woman in her thirties.
I think it happened gradually, the way you stop noticing a sound that plays on repeat after a period of time. What I do remember vividly is the absolute exhaustion. Being completely out of breath. The periods that arrived like a monthly reckoning. Somewhere along the way, I'd internalized the idea that this was simply what it meant to grow up as a woman—that discomfort was the price of admission.
So when things started to change for the worse, I did what I'd been conditioned to do: I pushed through. I told myself this was fine, this was normal, this was just life now. I kept pushing through even while my body was whispering that something was wrong.
But then it started screaming.
The Slow Collapse
My periods have always been heavy, but about two years ago, they crossed into a different territory entirely. I'm talking about a level of bleeding that made me rearrange my life around bathroom proximity. But even that wasn't the worst part. The worst part was the exhaustion.
Now, I've been lifting weights for a few years. I am fit. I know what tired feels like after a hard workout, after a long day, or after a bad night of sleep. This was completely different. This was a fatigue so profound it felt like my body was shutting down from the inside out.
I couldn't walk up the stairs in my own home without gasping for air at the top. Just standing up from the couch during my period left me winded, like I'd sprinted a mile. I felt like I was dying; that is genuinely what it felt like. I could tell my body was failing me in slow motion, and I had no clue as to why.
That's when I knew I needed to seek some help.
When "Normal" Becomes the Enemy
So, I did the responsible thing. I went to my primary care doctor and had my annual bloodwork done to see what was going on. The appointment lasted maybe fifteen minutes; there wasn't much conversation. No one asked me to describe what I was experiencing or how it was affecting my life. It felt transactional, like I was just another person being herded in and out of the office as fast as possible.
A few days later, my results appeared in my patient portal. Everything was in "normal” range… but no one called. My doctor didn’t follow up. No one took the time to walk through my results with me or help me understand why my levels came back “normal” while I was feeling like death every single month. And for a split second, I wondered if I was losing my mind. If maybe this crushing exhaustion was just what being a woman in her mid-thirties felt like, and everyone else had simply learned to live with it. But something in me refused to accept that; I knew I couldn’t keep feeling this way for a week every single month of my life.
“You know your body better than anyone else. If something feels off, it deserves investigation—even if your labs say you're ‘normal.’ Normal does not mean optimal. And optimal is what allows you to actually live, not just survive.”
The First Real Clue
Around that time, I came across Function Health—a company founded by Dr. Mark Hyman that offers comprehensive lab testing with over 160 biomarkers and an actual clinical review of your results. It’s not just a portal dump with checkmarks, but it provides actual analysis with next-step recommendations. It felt like a better use of my energy than continuing to bang my head against a system that (clearly) wasn't listening.
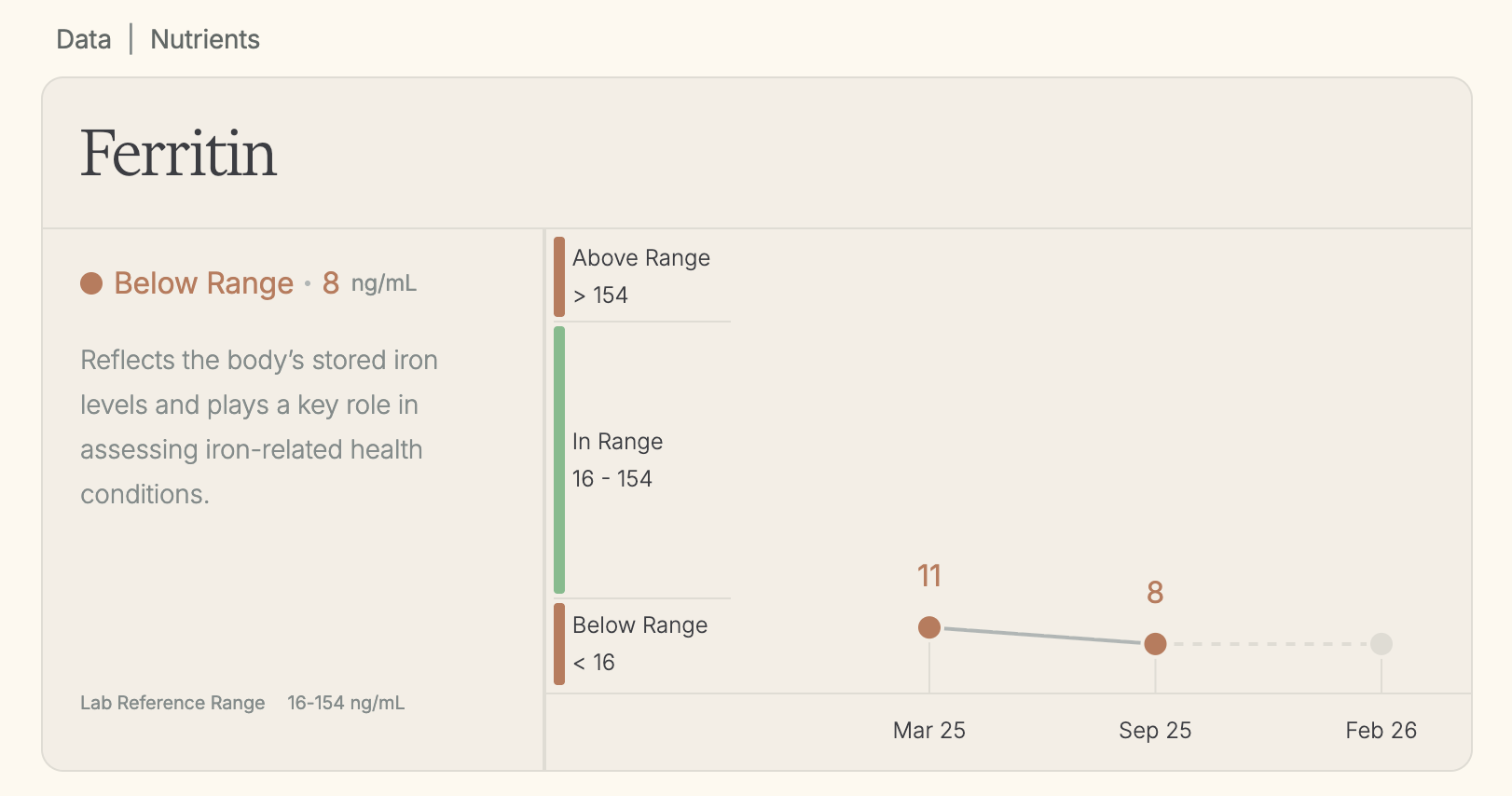
So after my lab appointments, when my Function results came back, I finally saw something that actually made sense. My ferritin level was 11.
Now, if you're not familiar with ferritin, here's what you need to know: first, it isn't always a standard part of basic routine blood work; Complete Blood Counts (CBCs) or Full Blood Counts (FBCs) that you might get from your primary care doctor’s annual bloodwork measure only up to about 20 or so biomarkers. Ferritin is also not the same as iron or hemoglobin; ferritin measures your body's iron storage—how much “reserve fuel” you have in the tank. And while different labs define "normal" differently (which is part of the problem), most experts agree that for menstruating women, ferritin should be closer to 50 or above to actually feel good.
Thankfully, Function’s lab tests include ferritin as one of the 160+ biomarkers measured. And at only 11, I was legitimately running on fumes.
Low ferritin can cause extreme fatigue, heavy periods, brain fog, dizziness, hair loss, shortness of breath, exercise intolerance, and feeling cold all the time. Basically, every single thing I'd been experiencing for a long time.
Suddenly, I didn’t feel crazy: I was just iron-deficient.
When the Fix Doesn't Stick
I brought my results to a functional medicine doctor I'd been seeing the year prior and asked the obvious question: what do we do to increase my levels?
Because my husband and I were hoping to start trying for a family in the next year or two, my doctor’s goal was to get my ferritin to at least 50. The plan was for me to get monthly iron injections, plus dietary changes and supplements.
So for the next five months, I drove across the city once a month to get a shot of iron in my muscle. And it was worth it. The injections were quick, and I could feel them working almost immediately. I had more energy. My periods were still heavy, but they weren't completely leveling me anymore. Around the three- or four-week mark, I could feel the effects start to fade, but by that time, it was almost time for my next injection appointment anyway.
When it came time to retest my labs in September 2025, I was so excited to see how much my injections had increased my levels. If my ferritin was 50 or higher, I knew my husband and I could begin trying for a baby the following spring and I wouldn’t have to worry about being iron-deficient while pregnant (NOT a good combo). So when my results came back, I couldn’t wait to open them.
But then I saw the number.
My ferritin had dropped even further: I went from 11 to 8.
I was legitimately shocked. Not because I felt worse—I actually felt better. But how was it possible that I'd been getting monthly iron injections for five months and my levels hadn’t stayed the same, but dropped more?
My Breaking Point
When I called my doctor, they explained what was happening: first, it was a good sign that I was feeling better with the injections. That told them my body was responding well to the extra iron. It was just, unfortunately, using every single bit of it immediately that there was nothing left to store. I was still running a deficit.
Their recommendation? Increase from once a month to twice a month.
And that's when I made the decision that their plan wasn't aggressive enough for me. I needed to go from 8 to 50 in a matter of months—not years. That timeline mattered. And what we were doing clearly wasn't going to get me there in the timeframe I wanted.
So I did something I hadn't realized I was allowed to do as a patient at the mercy of a medical doctor’s trained guidance.
I asked for a referral to a specialist, someone who I felt would be better equipped to help me and help me quickly. I asked for a referral to a hematologist.
“For decades, women's health has been underfunded, under-researched, and deprioritized. Many medical reference ranges are still based on male bodies. Which means it's often up to us to ask better questions, push for second opinions, and demand care that actually meets our needs.”
Finding Someone Who Actually Gets It
I found one of the best hematologists in my city at the Piedmont Cancer Institute (shoutout Dr. Jonas and Dr. Helms!) and got on their schedule as quickly as I could. From the moment they walked into the room, I knew I was in the right place.
Immediately upon entering the room, Dr. Jonas told me something I'll never forget: he said he loves treating iron deficiency patients because it's one of the few conditions where you can actually help people feel dramatically better, relatively quickly, and improve their quality of life. He explained that some bodies just need more iron than others—like cars that need oil changes more frequently. Depending on the cause (heavy periods, poor absorption, genetic reasons, diet, internal bleeding), your stores can quietly drain for years without you realizing it.
Given how depleted I was, he recommended iron infusions, while recommending I rule out a couple of other causes (internal GI bleeding, uterine fibroids causing severe heavy periods, etc.). Within a week of first seeing Dr. Jonas, I was scheduled to receive three infusions of IV iron sucrose (Venofer), 200 mg each session.
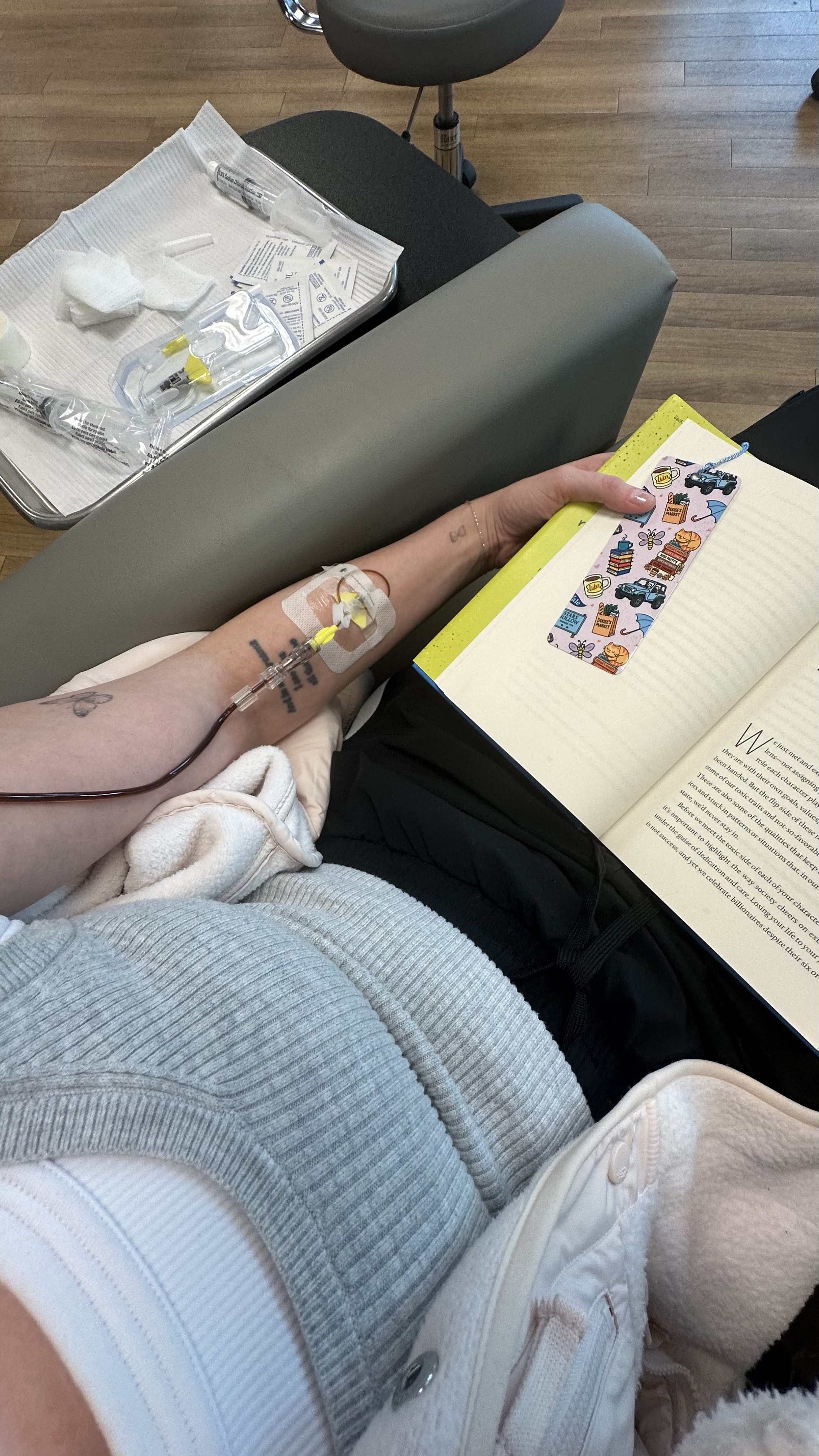
Iron infusion #3
My infusions were quick and painless. After each one, I didn't feel a lightning bolt of energy which I had read was the experience of others with iron deficiency. But after a few weeks, I could tell something had shifted a bit. I stopped feeling like my body was betraying me every single month. The bone-deep exhaustion lifted a bit. I could do things around the house or plan activities on or during my period that wouldn’t absolutely obliterate me. I could walk up my stairs without needing to catch my breath.
For the first time in years, I felt like I had some reserves.
The Proof
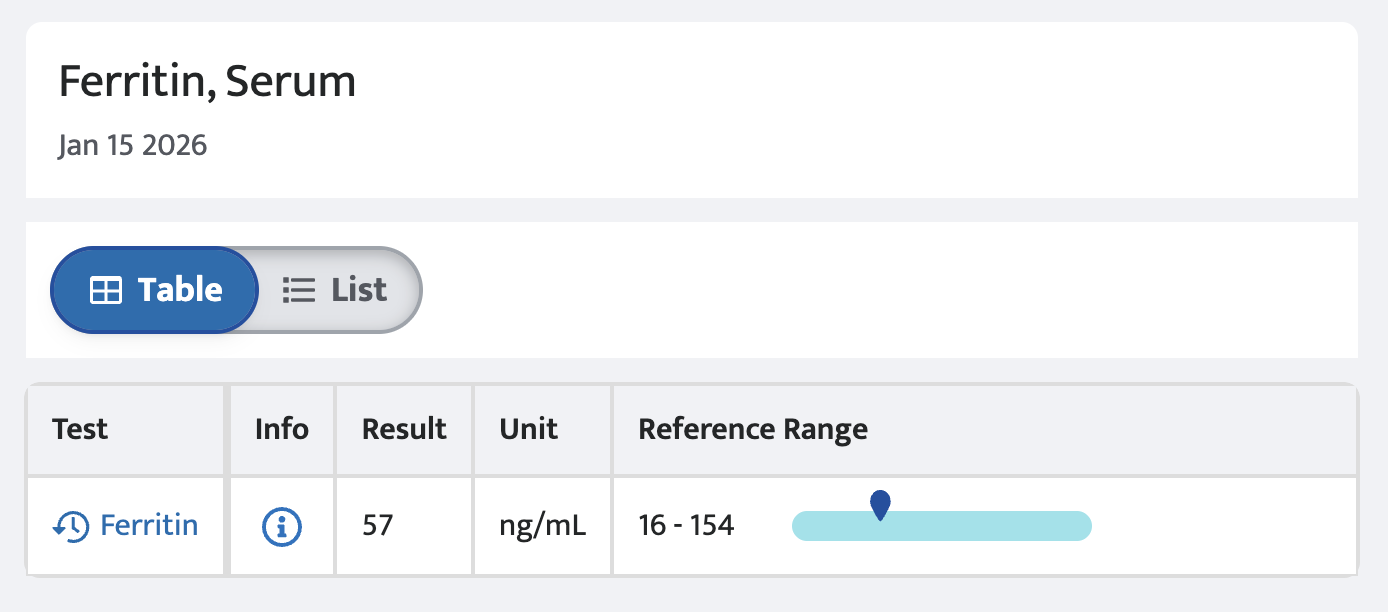
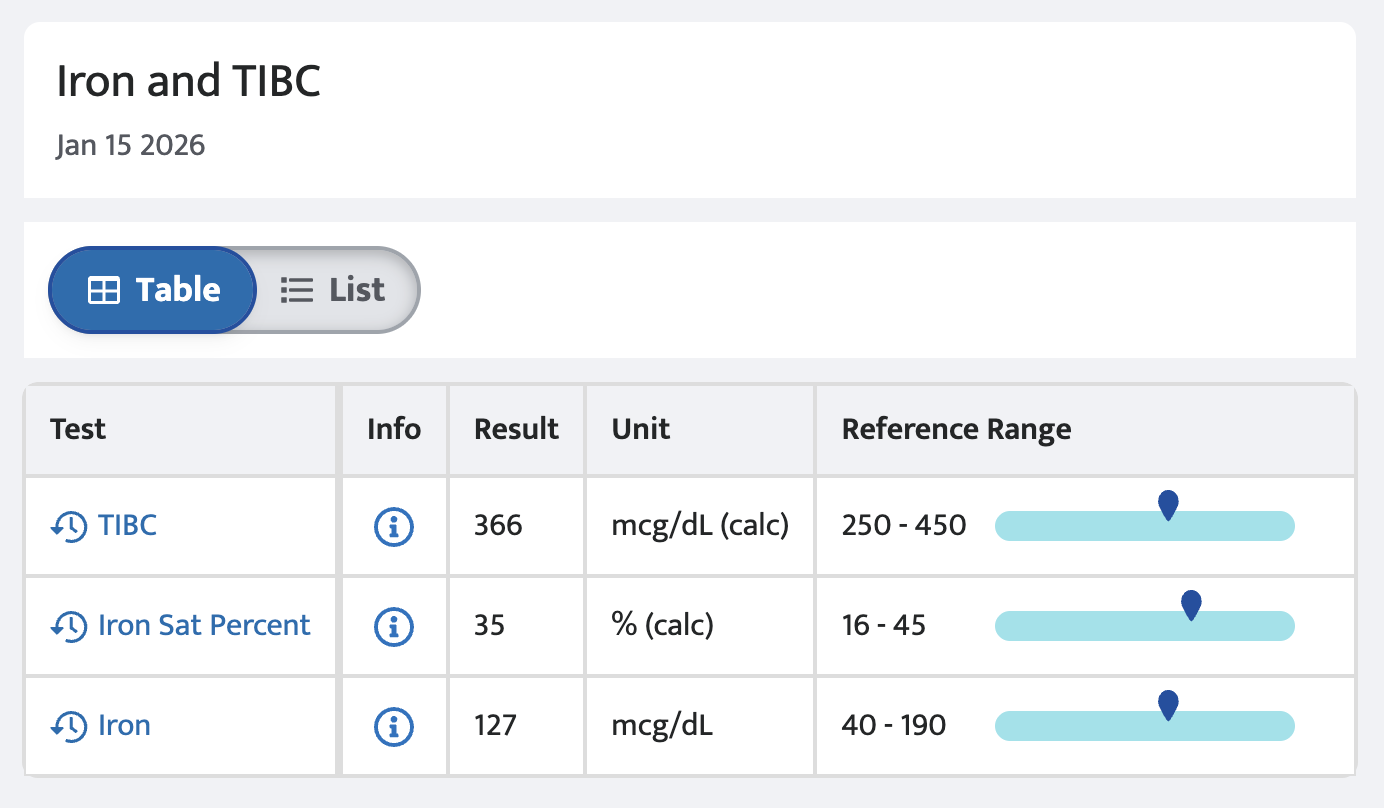
Six weeks later, I went back for follow-up labs. Ferritin is a biomarker that takes time to build — testing ferritin too soon after an infusion will yield inaccurate results. So last week, the second week of January 2026, I had my blood re-drawn for ferritin, hemoglobin, iron saturation, and more.
And— finally—my ferritin was 57.
I stared at the number on the screen and felt something I hadn't felt in a long time: complete relief. Not just because the number was higher, but because this proved my body finally had what it needed. My iron saturation and hemoglobin were in much healthier ranges, too.
As for next steps, I’ll go back to Dr. Jonas every six months to keep monitoring my levels. And if my body needs another "tune-up," we'll simply do infusions again. But probably most importantly out of all of this… I finally trust that I'm being taken seriously and that how I feel in my body matters.
What I Want You to Know
If you take nothing else from my story, please take this:
You know your body better than anyone else. If something feels off, it deserves investigation—even if your labs say you're "normal." Normal does not mean optimal. And optimal is what allows you to actually live, not just survive.
For decades, women's health has been underfunded, under-researched, and deprioritized. Many medical reference ranges are still based on male bodies. Which means it's often up to us to ask better questions, push for second opinions, and demand care that actually meets our needs.
Here's what helped me advocate for myself, and what might help you:
In the doctor's office, try saying:
"These symptoms are affecting my quality of life, even if my labs look normal."
"What additional testing or specialists could help us understand what's happening?"
"I'd like a referral for a second opinion."
At the end of the day, I hope you listen to your body. Ask questions. Do your research. Find your people—the doctors, the communities, the friends who will believe you when you say something is wrong.
And please remember: you are not difficult, dramatic, or overreacting for wanting to feel well. You are the most invested person in your own health. That matters more than any lab range, any dismissive appointment, any "everything looks normal" ever will.
When your body is trying to tell you something, it's always worth listening to.